It enables personalized treatment decisions with a comprenhensive diagnosis of coronary artery disease
Description of the work performed at University of Oxford, demonstrating that mediators released by an inflamed coronary artery cause changes in the size and composition of fat cells surrounding the artery
Post-hoc analysis of prospectively gathered outcome data from 3,912 participants in two cohort of approx. 2000 consecutive patients each, with up to 10 year-follow-up
After adjusting for all conventional risk factors, abnormal FAI is associated with 6-9X higher risk for fatal heart attacks
Biologic therapy was associated with a significant decrease in coronary inflammation in a cohort study of consecutive patients with moderate to severe psoriasis.
Patients not receiving therapy had no change.
Sub analysis of the CRISP-CT study with patients stratified based on the presence or absence of High-Risk Plaque features
In the absence of inflammation, HRP features are not associated with increased cardiac risk
Despite advancements in cardiovascular diagnostics and therapeutics over the last few decades, coronary heart disease is still the number one killer globally.
Conventional cardiac testing focuses on angina or detecting ischaemia whereas Coronary Artery Disease starts long before. Indeed, 2/3 of heart attacks occur in patients considered at low risk by conventional risk scoring cardiac testing, and 50% did not have any preceding symptoms.
It is well established that inflammation is not only a major driver of atherosclerosis, but also triggers plaque rupture. Hence it is considered a rational therapeutic target to reduce cardiovascular risk as shown in several randomized trials.
Apparently healthy persons without hyperlipidemia (low LDL) but with systemic inflammation (elevated hsCRP)
Primary end point:
First occurrence of myocardial infarction, stroke, arterial revascularization, hospitalization for unstable angina, or confirmed death from cardiovascular causes
Patients with previous myocardial infarction and residual systemic inflammation (elevated hsCRP)
Primary end point:
First occurrence of nonfatal myocardial infarction, nonfatal stroke, or cardiovascular death
Patients with a recent myocardial infarction (<30 days) who completed planned PCI and treated with intensive use of statins
Primary end point:
Composite of cardiovascular death, resuscitated cardiac arrest, myocardial infarction, stroke, or urgent coronary revascularization
Stable Patients with evidence of coronary disease by ICA or CCTA, or Calcium score> 400
Primary end point:
Composite of cardiovascular death, myocardial infarction, ischemic stroke, or ischemia-driven coronary revascularization
However, the benefits are only modest in unselected populations. With tests able to detect coronary inflammation, it becomes possible to provide precision treatment to patients, targeting the people who will benefit most, whilst preventing unnecessary costs and potentially harmful side-effects in people who will not benefit.
In the CRISP-CT Study, of ~4000 consecutive patients, abnormal FAI was associated with a 6-9x higher risk for fatal heart attacks, above-and-beyond all conventional risk factors (such as age, smoking, diabetes, high cholesterol).
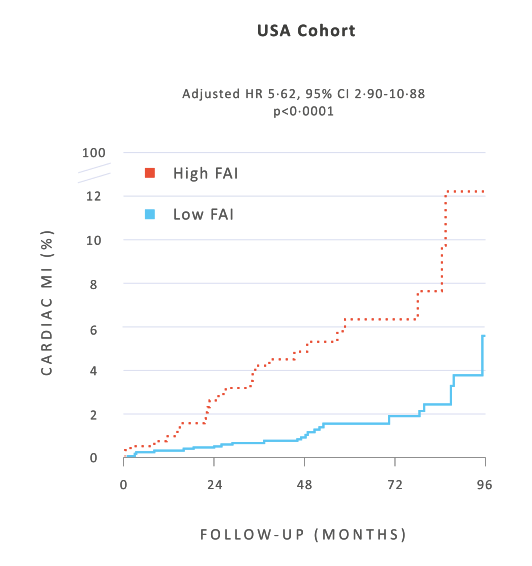
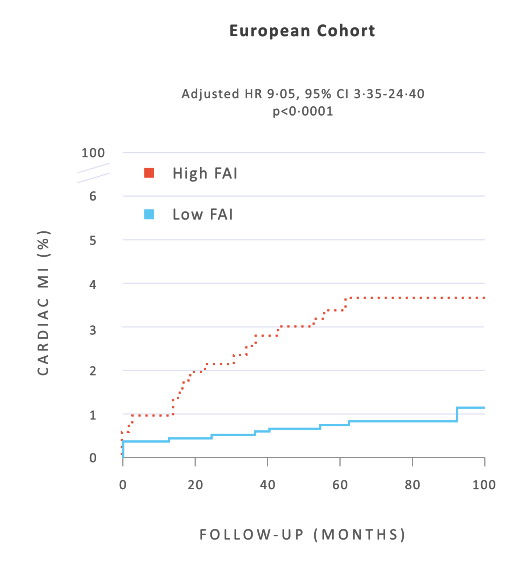
The striking predictive power of FAI was also independent of ‘high risk plaque features’, currently reported on CCTA scans.
The presence of high-risk plaque features does not predict increased risk in people who have a low FAI, whereas people with a high FAI have higher risk, even in the absence of high-risk plaque features.
Read all publications here